Channels
Special Offers & Promotions
UCLA Researcher Studies Neural Stem Cells on International Space Station
Research uses time-lapse imaging to study cell grow and development after exposure to space microgravity
When UCLA’s Dr. Araceli Espinosa-Jeffrey sent human brain cells into space, her goal was to gain a better understanding of how neural stem cells grow and develop in microgravity. That understanding is key to discovering more about the serious issues of intracranial hypertension affecting astronauts returning from space. The information may also one day be used to further cell replacement therapies for people with neurological disorders or neurological diseases. She and her research team needed access to dedicated microscopy equipment to conduct time sensitive 72-hour time lapse to capture images on proliferation and migration as cells re-adapted to terrestrial gravity as part of the study. They turned to ZEISS for a one-month loan of equipment, which was used to process samples flown on the International Space Station during SpaceX CRS-16.
Unique study investigates multiplication of nervous system cells in microgravity
Araceli Espinosa-Jeffrey, Ph.D., a research neurobiologist at the Semel Institute for Neuroscience and Human Behavior at UCLA, has had a longstanding interest in making more neural stem cells faster. Her initial interest was for their use in transplantation research. She had conducted experiments that observed a faster rate of cell growth in simulated microgravity (sim?µG) compared to that seen under standard Earth gravity conditions.
Believing that studies using microgravity will increase understanding of the brain in health and disease – in particular, to the discovery of new molecules and mechanisms impossible to unveil while in 1G – she sought and obtained funding from the National Aeronautics and Space Administration (NASA) to place an experiment using human brain cells aboard the International Space Station.
The experiment to test whether cell proliferation is increased in actual microgravity was managed by NASA’s Ames Research Center Space Biosciences Division. Originally scheduled for flight in SpaceX CRS-14, it was delayed to SpaceX CRS-16, a commercial resupply service mission to the International Space Station. The goal was to confirm and expand the results from the sim?µG microgravity experiments and learn more about cells in space microgravity, including the effects on different cell types.
NASA’s particular interest in funding the research was spurred by its desire to learn more about the role increased division of these cells in space may play in the intracranial hypertension (pressure inside the skull) observed during human spaceflight, which often does not normalize upon return to Earth. This type of intracranial pressure can cause vision problems, headaches, glaucoma, and other serious health problems, making it a significant obstacle to long-duration space exploration missions. NASA is hoping a better understanding of how central nervous system stem cells divide in microgravity could help lead to ways to protect astronauts from problems with intracranial pressure and design adequate preventive measures.
The work was also designed to investigate the effects of microgravity on the secretome of stem cells, which includes proteins important for cell-cell communication, function, and differentiation. The knowledge gained from the experiment will contribute to a better understanding of how stem cell growth is affected by gravity at the molecular level and may help advance neural stem cell technologies that might be used in wound healing, tissue regrowth, and organ culture.
When the cell types used in this study were cultured in sim?µG on the ground, they divided faster than cells cultured under normal gravity conditions. Studying the reasons why, and the mechanisms causing these cells to divide faster in microgravity, could pave the way to breakthroughs in stem cell production for cell replacement therapies.
Finding ways to generate more stem cells is urgent, because there is currently no way to quickly produce the large numbers of stem cells needed for the many cell replacement therapies that are showing such promise for people with neurological disorders or neurological diseases like multiple sclerosis or developmental disabilities.
In addition, using one’s own cells without grafting opens up the possibility that a neural stem cell donor could be his or her own recipient, eliminating any risks of rejection. Such an approach could be used for head and spinal injuries, as well as other cell replacement therapies. In addition to her work with NASA, Dr. Espinosa-Jeffrey would like to work on these issues with the Center for the Advancement of Science in Space, Inc. (CASIS), which is pursuing research on the effects of microgravity on cells to better study diseases and therapies aimed at prevention and treatment.
Experiment details
The NASA experiment, dubbed BioScience-04: The Impact of Real Microgravity on the Proliferation of Human Neural Stem Cells and Derived-Oligodendrocytes, launched in the Space-X 16 Dragon capsule in December 2018.
Two types of cells were studied – neural stem cells and oligodendrocyte progenitor cells. Neural stem cells produce all three major nervous system cell types: neurons, and the two kinds of cells that support neurons – astrocytes and oligodendrocytes. Neural stem cells also produce progenitor cells, which are like stem cells because they divide to produce new cells but are more limited because they cannot divide and produce new cells indefinitely. One kind of progenitor cell produced by neural stem cells is the oligodendrocyte progenitor cell, which become mature oligodendrocytes. Oligodendrocytes form electrical insulating membranes known as myelin sheaths that coil around neuronal axons, allowing signals to move along nerves at normal speeds, and making these cells vitally important to nervous system health.
Testing whether these important cells divide faster into two daughter cells in the microgravity environment of space, the experiment is helping scientists study the cell signaling pathways that determine cell function, proliferation, and differentiation.
The two cell types were sent to the International Space Station in cell culture hardware developed by Airbus-Kiwi, rented from Airbus, and then installed in the Space Technology and Advanced Research Systems (STaARS)-1 Experiment Facility, where the cells were given time to grow and divide. Dr. Espinosa-Jeffrey created the experiments and inspired the STaARS team to design the self-contained box, controlling and automating the culture media exchanges from Houston, TX, so astronauts would not have to invest time on this task.
The experiment had to deal with delays; splashdown was 39.3 days instead of 35 days originally anticipated. After splashdown, transport to Long Beach airport, and delivery to UCLA, the human neural stem cells were retrieved from the hardware, plated onto poly-d-lysine-coated flasks in a proprietary stem cell chemically defined medium, and allowed to recover from space flight. Researchers then began measuring how much the cells had divided while in space as well as after space flight and identifying the proteins secreted. This work is still in progress.
It was extremely important to begin analysis immediately, so there would be no chance of missing any changes to the cells. “It was important that we were able to show that cells behaved like in simulated microgravity, where some cells move slightly faster,” said Dr. Espinosa-Jeffrey. “Checking data from time-lapse images we could see that cells had proliferated post flight. This means that both the cells that came back and their progenies “remember” being in space. The daughter cells keep proliferating, but we do not yet know the mechanism by which this is happening.” The team is characterizing features that differ from their simulated microgravity studies.
Dedicated microscope resources needed for crucial time-lapse imaging
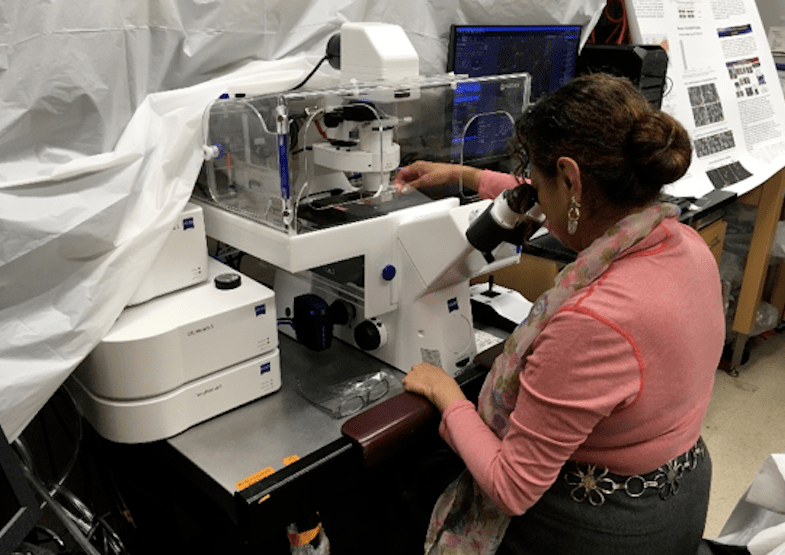
While Dr. Espinosa-Jeffrey was able to complete a portion of the analyses needed to study the brain cells that had been in space, other studies required specialized microscopy hardware to which she did not have sufficient access. In particular, there was a great deal of competition for equipment needed to perform time-lapse imaging to confirm the cells indeed proliferate more and provide data on all the properties they show.
To get the data on cells, time-lapse studies had to be performed over a period of at least 72 hours. During this time the cells had to be sustained in a controlled temperature and gas environment that is equivalent to what they would experience in a standard tissue culture incubator. The cells had to be kept at the temperature of the human body at in vivo conditions to mimic their native environment.
Given the risk of sample degradation over time and a potentially diminished ability to detect subtle effects of the spaceflight environment, completion of this analysis is time critical. “When the cells come back, there is no time to lose because you might miss subtle changes to cells,” explains Dr. Espinosa-Jeffrey. It was also extremely important to have dual stages so everything could be placed in parallel.
To meet the need for dedicated microscopy resources, Dr. Espinosa-Jeffrey requested and was granted a one month loan of a complete Cell Observer system from ZEISS Research Microscopy Solutions. Equipment identified as critical to her study included the ZEISS Axio Observer 7 fully motorized inverted research microscope (equipped with Definite Focus 2); ZEISS Axiocam 506 monochrome camera with ZEISS ZEN software; and ZEISS Full Incubation XL chamber for Temperature and CO2 control with motorized scanning stage.
According to Dr. Espinosa-Jeffrey, the Definite Focus 2 feature was vital to the experiment because it allows researchers to maintain focus position for long periods of time – irrespective of temperature changes, thermal drift, or mechanical drift. This ability to maintain focus for long periods of time is critical for extended time lapse studies. Using a motorized scanning stage, she was able to mark six to eight positions and xyz location using ZEISS tiles and positioning software. Then she started the experiments, acquiring images every 10-15 minutes at each position, and repeating for the 72 hour duration. From the position list developed she was able to create several time lapse movies that show cells growing and proliferating as well as other features such as migration.
Dr. Espinosa-Jeffrey has used ZEISS equipment extensively in Mexico City, France and the United States. “I love the optics of the instruments and I find customer support and training to be excellent. If you have a situation, they try to help you the most possible. They even try to help with other older microscopes to keep them working as long as possible.”
Further studies needed to design effective countermeasures
The proliferation of neural stem cells in space must be studied in more detail to determine the possible relationship to the visual impairment and intracranial pressure syndrome exhibited by astronauts in space and upon their return to Earth. Learning more is essential to be able to design effective countermeasures for astronauts working onboard the International Space Station and for long-term space travel.
The next phase of the work will be performed on SpaceX-21, a commercial resupply service mission to the International Space Station using the new Dragon 2 spacecraft, planned for October 2020.
References
- NASA, Our Experiments, https://www.nasa.gov/spacebio/our-experiments, retrieved 4/21/2020.
- Simulated microgravity enhances oligodendrocyte mitochondrial function and lipid metabolism, Araceli Espinosa?Jeffrey Kevin Nguyen Shalini Kumar Ochiai Toshimasa Ryuji Hirose Karen Reue Laurent Vergnes Jason Kinchen Jean de Vellis, 28 September 2016. https://onlinelibrary.wiley.com/doi/abs/10.1002/jnr.23958
- NASA, About Bioscience-04. https://www.nasa.gov/ames/research/space-biosciences/bioscience-4-spacex-16, retrieved 4/21/2020.
- Cepeda, C.; Vergnes, L.; Carpo, N.; Schibler, M.J.; Bentolila, L.A.; Karouia, F.; Espinosa-Jeffrey, A. Human Neural Stem Cells Flown into Space Proliferate and Generate Young Neurons. Appl. Sci. 2019, 9, 4042.
- NASA Space Biology Grant: NNX15AB43G; the Cell, Circuits and Systems Analysis Core is supported by the NIH (Grant U54HD087101)
- Espinosa-Jeffrey A, Paez PM, Cheli VT, Spreuer V, Wanner I, de Vellis J. Impact of simulated microgravity on oligodendrocyte development: implications for central nervous system repair. PLoS One. 2013;8 (12):e76963. Published 2013 Dec 4. doi:10.1371/journal.pone.0076963 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3850904/
Additional Notes:
ZEISS team members who supported the project:
- Mark Mobilia – Account Manager for UCLA
- Dr. Neeraj Gohad – Life Sciences PASS Manager, West
- Dr. Ben Ng – Field Applications Scientist
- Kevinne Aguilar – Local Service Engineer
- Stefan Gross – Regional Sales Manager West, US
- Tanya Mahboob – Demonstration Inventory Coordinator
Scott Olenych, PhD, Product Marketing Manager – Life Science Automation and WF, ZEISS Research Microscopy Solutions
Media Partners