Channels
Special Offers & Promotions
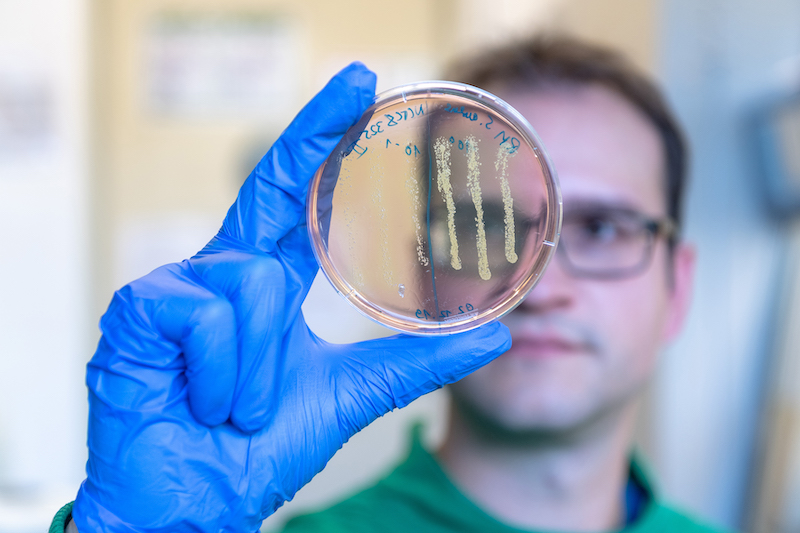
From cancer medication to antibiotic
Modified cancer drug effective against multi-resistant bacteria
Antibiotic-resistant bacteria are increasingly the source of deadly infections. A team of scientists from the Technical University of Munich (TUM) and the Helmholtz Center for Infection Research (HZI) in Braunschweig have now modified an approved cancer drug to develop an active agent against multidrug-resistant pathogens.
The methicillin-resistant Staphylococcus aureus (MRSA) is the source of severe and persistent infections. Some strains are even resistant to multiple antibiotics. There is consequently an urgent need for new drugs effective against MRSA infections.
"The industrial development of new antibiotics is stalling and not keeping pace with the spread of antibiotic resistance. We urgently need innovative approaches to meet the need for new infection therapies that do not lead directly to renewed resistance," says Prof. Eva Medina, director of the HZI Infection Immunology Research Group.
New antibiotic development strategies
One promising strategy is to test the potential effect of approved drugs on bacteria. “Our focus was on a class of human proteins, called kinases, which have many inhibitors to begin with," explains study leader Stephan Sieber, professor of organic chemistry at TUM.
In this vein, the researchers chemically modified the active ingredient sorafenib, a cancer drug that is effective against MRSA, to achieve a stronger antibiotic effect. This led to the development of PK150, a molecule ten times more effective against MRSA than the original substance.
Multiple attacks prevent the development of resistance
The potent new agent targets various unconventional structures within the bacteria. Two targets were investigated in greater detail: For one, PK150 inhibits an essential protein involved in bacterial energy metabolism. For another, it acts on the cell wall.
In contrast to previously known antibiotics such as penicillin and methicillin, which interfere with cell wall formation, PK150 acts indirectly. It knocks the protein production in bacteria off kilter. As a result, the bacteria release more proteins that control the cell wall thickness to the outside, causing the cells to burst.
In mice, PK150 has proven to be effective against MRSA in a variety of tissues. While staphylococci rapidly develop resistance to other antibiotics, the researchers did not observe the development of any resistance to PK150.
Effectiveness against biofilms and persisters
Eva Medina and Dr. Katharina Rox, a pharmacologist from the Department of Chemical Biology at HZI, showed that PK150 has favorable pharmacological properties. It can be administered as a tablet, for example, and remains stable in the body for several hours. "As a result of the chemical changes to the molecule, PK150 no longer binds to human kinases, but acts very specifically against bacterial targets," says Sieber.
And PK 150 has another benefit: "MRSA infections are very often chronic, as the bacteria can become dormant. PK150 even kills these, as well as germs protected in biofilms," says Prof. Dietmar Pieper, head of the HZI research group "Microbial Interactions and Processes".
In the context of the aBACTER project, Prof. Sieber's team is now further optimizing PK150 to enter the clinical development phase.
Publication:
Philipp Le, Elena Kunold, Robert Macsics, Katharina Rox, Megan C. Jennings, Ilke M. Ugur, Maria Reinecke, Diego Chaves-Moreno, Mathias W. Hackl, Christian Fetzer, Franziska A. M. Mandl, Johannes Lehmann, Vadim S. Korotkov, Stephan M. Hacker, Bernhard Kuster, Iris Antes, Dietmar Pieper, Manfred Rohde, William M. Wuest, Eva Medina, Stephan A. Sieber
Nature Chemistry, Dec. 16, 2019 – DOI: 10.1038/s41557-019-0378-7
Additional information:
The work was funded by the European Community (via the European Research Council (ERC) and the CHEMMINE research program), the German Research Foundation (DFG) within the Cluster of Excellence Center for Integrated Protein Science Munich (CIPSM) and the SFB 1035 Collaborative Research Center, the Chemical Industry Fund, the Boehringer Ingelheim Fund, the German Center for Infection Research (DZIF), the National Science Foundation (NSF) and the National Institute of General Medical Sciences (the latter two, USA). The aBACTER project is funded by the German Federal Ministry of Education and Research (BMBF) as part of the VIP + program.
In addition to the Chair of Organic Chemistry, the Chair of Proteomics and Bioanalytics, and Radiochemistry Munich of the TUM, various working groups of the Helmholtz Center for Infection Research, the German Center for Infection Research, the German Cancer Research Center (DKFZ), Temple University (Philadelphia, USA), and Emory University (Atlanta, USA) participated in the research. Stephan Sieber is also scientifically associated with the Helmholtz Institute for Pharmaceutical Research Saarland (HIPS), an HZI site in cooperation with the University of Saarland, and the Institute for Advanced Study of the TUM.
The Technical University of Munich (TUM) is one of Europe’s leading research universities, with around 550 professors, 42,000 students, and 10,000 academic and non-academic staff. Its focus areas are the engineering sciences, natural sciences, life sciences and medicine, combined with economic and social sciences. TUM acts as an entrepreneurial university that promotes talents and creates value for society. In that it profits from having strong partners in science and industry. It is represented worldwide with the TUM Asia campus in Singapore as well as offices in Beijing, Brussels, Cairo, Mumbai, San Francisco, and São Paulo. Nobel Prize winners and inventors such as Rudolf Diesel, Carl von Linde, and Rudolf Mößbauer have done research at TUM. In 2006, 2012 and 2019 it won recognition as a German "Excellence University." In international rankings, TUM regularly places among the best universities in Germany.
Media Partners