Channels
Special Offers & Promotions
Four-fold difference in antibiotic consumption across the WHO European Region
A new report (1) published in The Lancet Infectious Diseases on 20 March 2014, is the first to release data on total antibiotic consumption for countries outside the European Union (EU).
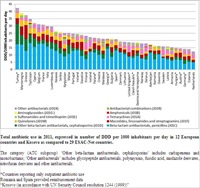 The data (from 2011) indicate an almost fourfold difference between the lowest and the highest antibiotic users among 42 countries and regions in the WHO European Region (within and outside the EU), and provide a clear picture of the use of different groups of antibiotics.
The data (from 2011) indicate an almost fourfold difference between the lowest and the highest antibiotic users among 42 countries and regions in the WHO European Region (within and outside the EU), and provide a clear picture of the use of different groups of antibiotics.
“Antibiotic overuse and misuse are the most important factors in creating resistance. That is why mapping consumption is the first step in identifying and tackling this growing public health problem,” says Ms Zsuzsanna Jakab, WHO Regional Director for Europe. “As antibiotic resistance respects no borders, the work we are doing in the non-EU part of the Region adds enormous value to existing EU data and action.”
“Until now there were no reliable data on antibiotic use in non-EU countries in the WHO European Region,” says Professor Herman Goossens of the University of Antwerp and lead investigator of the study. “Our results will raise awareness of inappropriate antibiotic use and will help these countries to develop quality indicators of antibiotic use. I invite policy-makers to develop national action plans, which can be assessed if this newly established surveillance system is continued and expanded to other countries of the Region.”
The study, carried out by the WHO Regional Office for Europe and the University of Antwerp with the support of the Ministry of Health, Welfare and Sport of the Netherlands, collected and analysed wholesale data from six south-eastern European and seven central Asian areas and countries. This complements the work that is carried out in 29 countries (the 28 EU Member States plus Norway) participating in the European Surveillance of Antimicrobial Consumption Network (ESAC-Net) of the European Centre for Disease Prevention and Control (ECDC). In 2011, the 53 Member States in the WHO European Region adopted a comprehensive European strategic action plan on antibiotic resistance, including a commitment to strengthen surveillance systems to monitor the use of antibiotics.
Key results
Antibiotic consumption differed significantly among the participants in the study. When compared to EU countries, some study participants ranked as top consumers (Montenegro, Tajikistan and Turkey) and others as low consumers (Armenia, Azerbaijan, Belarus and Bosnia and Herzegovina). Low antibiotic use may reflect underuse due to limited access to medicines for significant parts of the population. In Belarus, for example, this might be the consequence of a policy for universal access to health services.
Penicillins were the most frequently used by all participants, with a generally high use of broad-spectrum penicillin (amoxicillin and ampicillin), especially in the newly independent states (NIS). Participants in south-eastern Europe consumed high volumes of first-generation cephalosporins, comparable to use in northern EU countries. Montenegro and Serbia in particular used the long-acting macrolide azithromycin. Remarkably high use of parenteral antibiotic treatment was observed in all the NIS.
The study provides a foundation for action to address antimicrobial resistance in the participants. For example, the Turkish Government has already taken steps to reduce high antibiotic consumption through an action plan for 2013–2017.
Prescriptions and consumption patterns
Comparisons allow a better understanding of antibiotic prescription and consumption patterns. In particular, the study shows some disturbing patterns.
- Total antibiotic consumption is too high. This indicates that antibiotics are overprescribed and that the population has easy access to antibiotics in pharmacies through over-the-counter sales. Massive regulatory action would be needed to change this.
- Wide-spectrum antibiotics are overused. This suggests that they are overprescribed, diagnostic tools are inappropriate and both prescribers and population have limited knowledge of antimicrobial resistance;
- The seasonal fluctuations in consumption indicate that antibiotics are improperly used to treat seasonal viral infections.
- Particular brands of antibiotics are overused and misused. This may result from marketing by the pharmaceutical industry, as well as insufficient knowledge in prescribers and the general public.
- In contrast, however, many study participants face challenges in gaining access to important antibiotics, such as those to treat multidrug and extensively drug-resistant tuberculosis and other multidrug-resistant bacteria.
“These new findings represent a landmark in advancing knowledge on antibiotic consumption,” concludes Dr Hans Kluge, Director of the Division of Health Systems and Public Health at the WHO Regional Office for Europe. “We are confident that they will encourage regulatory action at the national and European levels on the provision, prescription, consumption and dispensing of antibiotics.”
Other non-EU countries are collecting data and plan to join the initiative.
Media Partners